 |
- If you cannot see edges, use general anesthesia
- If you can see edges, use local or block
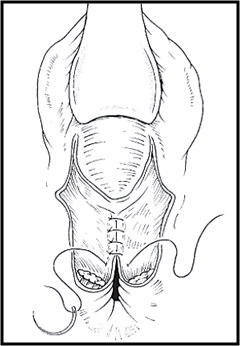
- Repair rectal mucosa with 3-0 or 4-0 interrupted sutures
- Close fascial layer
- Close sphincter with interrupted 2-0
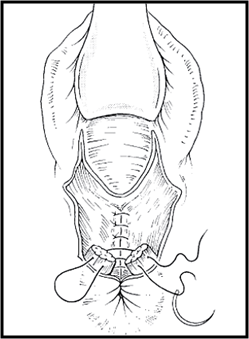
- During repair, use multiple rounds of antiseptic wash
- Change gloves
- Repair vaginal mucosa, perineal muscles, skin
|
 |