BURN FIRST AID
- Stop burning process by removing clothing, irrigating burns
- Use cool running water to reduce temperature of burn
- Extinguish flames by allowing patient to roll on ground, by applying a blanket, by using water or other fire-extinguishing liquids
- In chemical burns, remove or dilute chemical agent by irrigating with large volumes of water
- Wrap patient in clean cloth or sheet, transport to nearest appropriate medical facility
- Do not start first aid before ensuring your own safety (switch off electricity, wear gloves for chemicals, etc.)
- Do not apply paste, oil, turmeric or raw cotton to burn
- Do not apply ice, may deepen injury
- Avoid prolonged cooling with water, will lead to hypothermia
- Do not open blisters until topical antimicrobials can be applied at health care facility
- Avoid application of topical medication until patient has been placed under appropriate medical care
ACUTE BURN MANAGEMENT
- Stop the burning
- ABCDE's
- Determine percentage area of burn
- Good IV access, early fluid replacement
- Adequate pain control essential
- Severity of burn determined by:
- - Burned surface area
- - Depth of burn
- - Other considerations
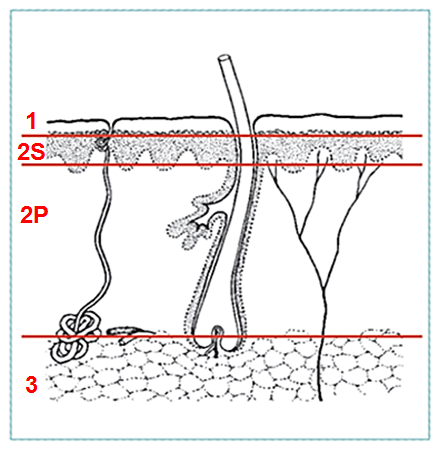
ACUTE BURNS
- 1st degree: superficial
- epidermis and upper dermis
- 2nd degree: partial thickness
- Superficial partial thickness (S)
- Deep partial thickness (P)
- - Penetrates deep in dermis
- - Skin grafting recommended
- 3rd degree: full-thickness
- Destroy all epidermal and dermal elements
- Always use skin grafts
- Most are mixed depth
|
 |
ACUTE BURN MANAGEMENT
Airway: beware of inhalation, rapid airway compromise
Breathing
Circulation: fluid replacement
Disability: compartment syndrome
Exposure: percentage area of burn
Morbidity and mortality rises with increased burn surface area or with increased age; even small burns may be fatal in elderly
ACUTE BURNS
| Depth of Burn |
Characteristics |
Cause |
| First degree |
- Erythema
- Pain
- Absence of blisters
|
|
Second degree
- superficial partial thickness
|
- Red or mottled
- Flash burns
- Blisters
- painful
|
|
| Second degree
|
- Pale
- Reduced sensation
- With or without blisters
|
|
| Third degree
|
|
- Fire
- Electricity or lightning
- Prolonged exposure to hot liquids/objects
|
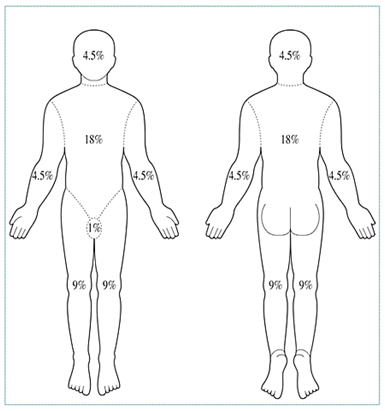
ESTIMATION OF BURN AREA: �Rule of 9's
- Count non-superficial burns (2nd degree and 3rd degree)
- The patient’s hand is approximately 1% of body surface area.
|
 |
ESTIMATION OF BURN AREA: CHILDREN
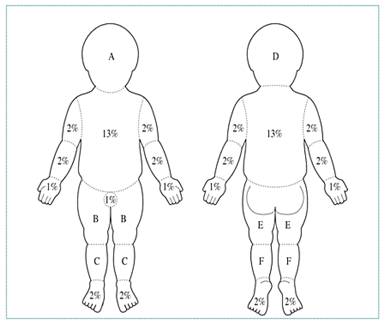 |
| Area |
By Age in Years |
| |
0 |
1 |
5 |
10 |
| Head (A/D) |
10% |
9% |
7% |
6% |
| Thigh (B/E) |
3% |
3% |
4% |
5% |
| Leg (C/F) |
2% |
3% |
3% |
3% |
|
FLUID RESUSCITATION
Necessary for burns
- >15% of total body surface area (TBSA) in adults
- >10% of total body surface in children
- Use Ringer’s lactate or normal saline
The fluid requirement for the first 24h can be calculated
2 - 4 ml x body weight in kg x %TBSA
- Give half in the first 8h and remainder in the next 16h
- Children also need maintenance fluids with glucose
- Monitor urine output and adjust iv fluids
ACUTE BURN MANAGEMENT
- Focus care on rapid healing, infection prevention
- If small area: immerse in cold water 30 minutes to reduce oedema, tissue damage
- Tetanus toxoid
- Remove broken, tense or infected blisters
- Excise adherent necrotic tissue
- Gently cleanse burn with 0.25% (2.5 g/l) chlorhexidine solution, 0.1% (1 g/l) cetrimide solution, or another mild water-based antiseptic
- Maintain good nutrition: very high metabolic demands due to burns
- Change burn dressing daily or as often as necessary to prevent seepage through dressing
- On each dressing change, remove any loose tissue
- Inspect wounds: discoloration, hemorrhage may indicate developing infection.
- Cellulitis in surrounding tissue is an indicator of infection
- Fever is not a useful sign; may persist until burn healed
- Administer topical antibiotic chemotherapy daily: Silver nitrate (0.5% aqueous) cheapest, apply with occlusive dressings, does not penetrate eschar
- Use silver sulfadiazine (1% miscible ointment) with single layer dressing; has limited eschar penetration, may cause neutropenia
- Mafenide acetate (11% miscible ointment) used without dressings; penetrates eschar but causes acidosis
- Alternating these agents is an appropriate strategy
Serious burn requiring hospitalization:
- Greater than 15% burns in adult
- Greater than 10% burns in child
- Any burn in very young, elderly, infirm
- Full thickness burns
- Burns of special regions: face, hands, feet, perineum
- Circumferential burns
- Inhalation injury
- Associated trauma or significant pre-burn illness: e.g. diabetes
- Treat burned hands with special care to preserve function
- Cover hands with silver sulfadiazine, place in loose polythene gloves or bags secured at wrist
- Elevate hands first 48 hours, then start hand exercises
- At least once a day, remove gloves, bathe hands, inspect burn, reapply silver sulfadiazine, gloves
- If skin grafting necessary, consider treatment by specialist after healthy granulation tissue appears
ACUTE BURN MANAGEMENT: �Healing phase
- Burn depth and surface involved influence duration of healing phase
- Without infection, superficial burns heal rapidly
- Apply split thickness skin grafts to full-thickness burns after wound excision or appearance of healthy granulation tissue
- Plan to provide long term care to patient
- Burn scars undergo maturation
- First red, raised, uncomfortable
- Frequently become hypertrophic, form keloids,
- Although soften, fade with time; can take up to two years
ACUTE BURN MANAGEMENT: Nutrition
- Energy, protein requirements extremely high due to the catabolism of trauma, heat loss, infection, demands of tissue regeneration
- If necessary, feed patient through nasogastric tube to ensure adequate energy intake
- Anemia and malnutrition prevent burn wound healing, result in failure of skin grafts
- Eggs, peanut oil are good, locally available supplements
ACUTE BURN MANAGEMENT IN CHILDREN
- ABCDE – consider respiratory injury
- Use ringer's lactate or normal saline for resuscitation
- Add maintenance fluids, glucose to avoid hypoglycemia
- Admit all children
- with burns >10% of body and
- those involving face, hands, feet, perineum
- circumferential
- Prevent infections with topical antibiotics.
- Prevent contractures by passive mobilization and splinting
- Scars cannot expand to keep pace with growth, may lead to contractures
- Arrange for early surgical release of contractures before interfere with growth
- Burn scars on face lead to cosmetic deformity, ectropion, contractures about lips
- Ectropion can lead to exposure keratitis, blindness; lip deformity restricts eating, mouth care
- Consider specialized care (referral) as skin grafting insufficient to correct facial deformity
- Pain control, especially during procedures
- Tetanus vaccination
- Nutrition
- Begin feeding as soon as practical
- Need high caloric diet
- Burn contractures
- - Prevent by splinting flexor surfaces, passive mobilization of involved areas
- Physiotherapy and rehabilitation
- Begin early, continue throughout burn care